Menopause & Bone Health- The Overview

Menopause is a natural and significant phase in a woman’s life, marking the end of her reproductive years. While symptoms like hot flashes, mood changes, and sleep disturbances often get the most attention, one of the most important and sometimes overlooked changes happening during menopause is its impact on bone health. Understanding how menopause affects your bones, why it happens, and what you can do about it is essential for maintaining long-term strength, mobility, and quality of life.
Why Bone Health Matters During Menopause
Bones may seem solid and unchanging, but they are actually living tissue that continually regenerates. Throughout life, the body balances two processes, breaking down old bone and building new bone. Until about age 30, your body builds more bone than it loses, but after that point, bone density naturally begins to decline.
When menopause arrives, typically between ages 45 and 55, the gradual decline can accelerate. The key reason behind this shift is the drop in estrogen levels. Estrogen is a hormone that plays a vital role in maintaining bone density. It helps regulate bone turnover, ensuring that bone breakdown doesn’t outpace bone rebuilding. Once estrogen levels fall, this balance is disrupted.
The result? Women can lose up to 20% of their bone density in the five to seven years after menopause. This rapid loss can significantly increase the risk of osteoporosis, a condition characterized by brittle bones and a higher likelihood of fractures.
The Role of Estrogen in Bone Health
To understand menopause’s effect on bone health, it’s helpful to look at what estrogen does for your skeletal system.
Slows bone resorption (the natural process of breaking down old bone)
Supports calcium absorption from the diet
Helps maintain bone remodelling balance
Contributes to muscle mass maintenance, indirectly supporting the bones
When estrogen declines, bone resorption speeds up, and the body may struggle to absorb enough calcium. Bones become weaker, more porous, and more susceptible to fractures, especially in the spine, hips, and wrists.
Osteopenia vs. Osteoporosis
Not all bone loss leads immediately to osteoporosis. Many women first experience osteopenia, a condition where bone density is lower than normal but not low enough to be considered osteoporotic.
Osteopenia is a warning sign. With the right lifestyle changes and interventions, progression can often be slowed or even prevented.
Osteoporosis involves more severe bone loss and carries a much higher risk of fractures, even from minor falls or everyday movements.
Because bone loss during and after menopause is often silent, many women don’t realize they’re at risk until a bone density scan (DEXA scan) or a fracture reveals the issue.
Risk Factors Beyond Menopause
While falling estrogen levels are the main driver of bone loss, other factors can influence your risk
Genetics- A family history of osteoporosis increases your risk.
Nutrition- A diet low in calcium, vitamin D, or protein weakens bones.
Lifestyle- Smoking, excessive alcohol consumption, and physical inactivity accelerate bone loss.
Body Size- Women with smaller frames may have lower starting bone mass.
Medical Conditions Thyroid disorders, autoimmune diseases, and long-term steroid use can affect bone strength.
Understanding your risk factors can help you take action earlier and more effectively.
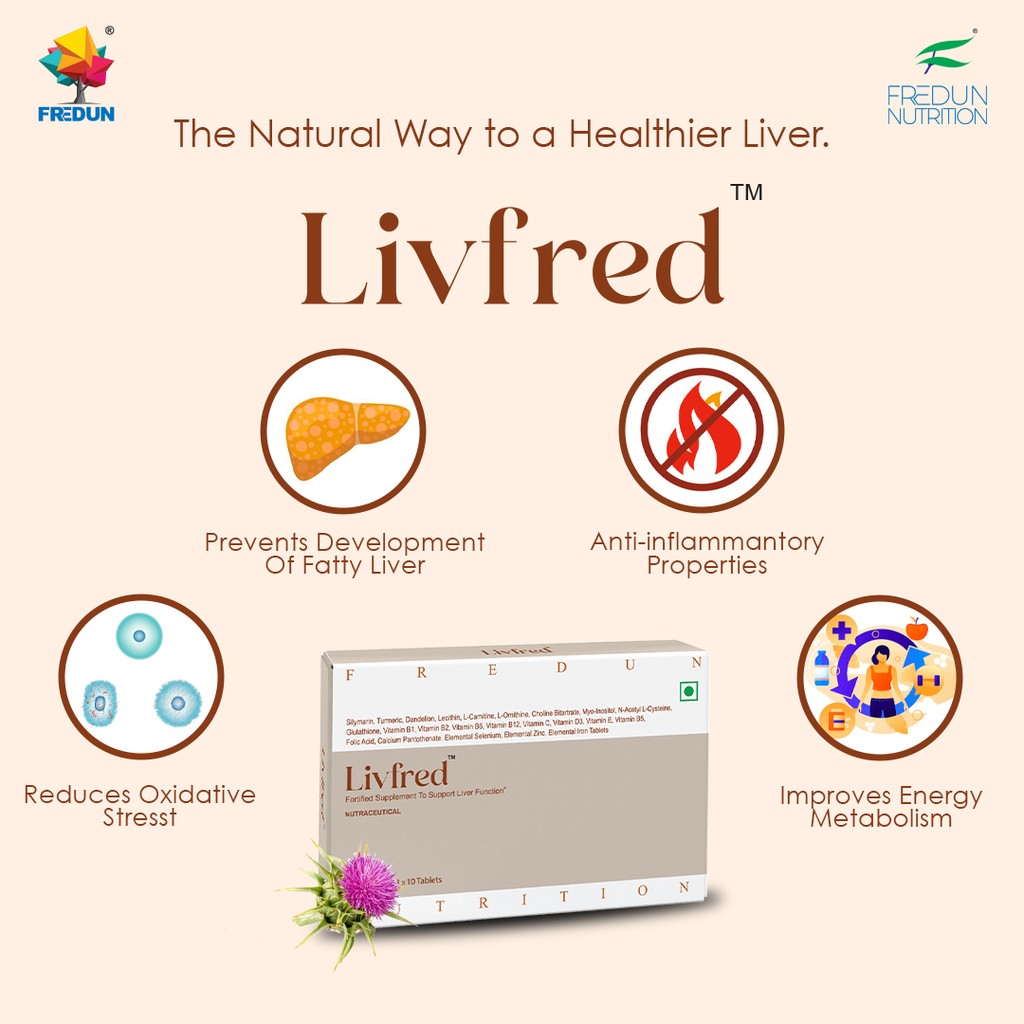
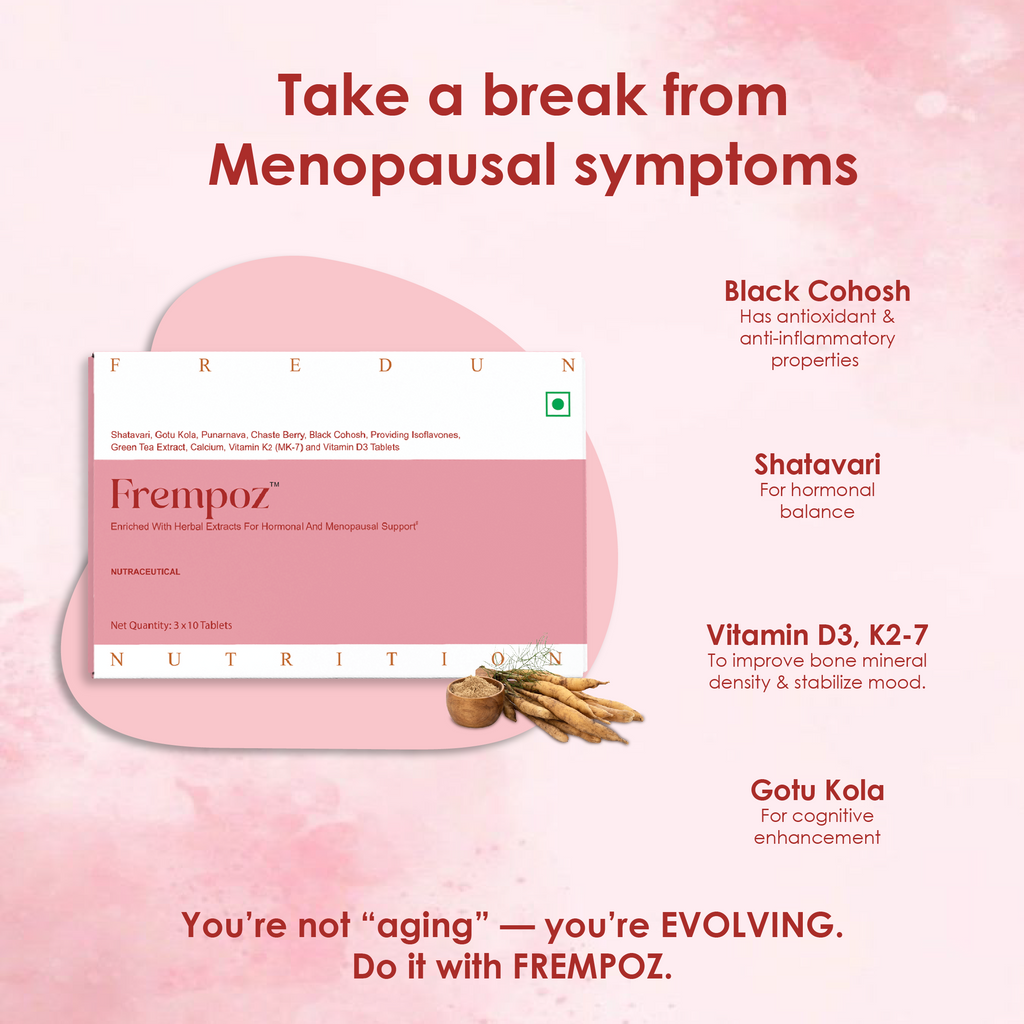
Why Choose FREMPOZ?
FREMPOZ alleviates physical and psychological symptoms of menopause
Enriched with phytoestrogens & isoflavones
SHATAVARI- contains phytoestrogenic compounds that bind to the estradiol receptor& helps to reduce postmenopausal estradiol deficiency contributes to to sarcopenia and osteoporosis.1
Improves muscle function, potentially mediated by improvements in myosin contractility.1
GOTU KOLA- For cognitive enhancement. Alleviates symptoms of anxiety and promotes relaxation. Reduces headache & body ache.2
PUNARNAVA- Helps to reduce old age anemia in patients above 50 years.9
CHASTE BERRY EXT.- For female reproductive disorders, including menstrual disorders (amenorrhea, dysmenorrhea), corpus luteum insufficiency, hyperprolactinemia, infertility & menopause.2
BLACK COHOSH- Provides an antioxidant, anti-inflammatory, anti-apoptotic action.3
Alleviates menopausal distress, post-menopausal-related hot flashes, anxiety, and cognitive dysfunction in adult women by its estrogenic activity.3
Reduces depression, and the possibility of providing protection against bone loss.3
Treats dry mouth which increases after menopause.3
ISOFLAVONES (TRIFOLIUM PRATENSE)- plant-based chemicals that produce estrogen-like effects in the body which relieves hot flushes and menopausal symptoms.4
GREEN TEA EXT.- Decreases lipid profile in postmenopausal women.5
CALCIUM- Significantly prevents early postmenopausal bone loss from the femoral neck and improves calcium balance in recently postmenopausal women.6
VITAMIN K2-7- Plays an important role in the maintenance and improvement of bone mineral density (BMD) and is beneficial and safe in the treatment of osteoporosis for postmenopausal women.7
VITAMIN D3- Helps to stabilize emotions and moods.8
Looking Ahead- Thriving Beyond Menopause
Menopause is a transition, not an ending, and with the right information, women can navigate it with confidence. Bone health is a critical piece of the puzzle, affecting your strength, mobility, and independence for decades to come.
By understanding the changes happening in your body and taking practical steps, such as nutritious eating, regular exercise, medical guidance, and self-care, you can preserve bone density, reduce your risk of fractures, and continue to live an active, vibrant life long after menopause.
Your bones support you every day. Menopause is the perfect time to start supporting them in return.